Dentin Implants Surface
The implant surface is key in achieving optimal Osseointegration. It is well documented that the surface characteristics of implanted materials can influence the healing and growth of tissues adjacent to the implant surface.
Current trends in clinical dental implant therapy include use of endosseous dental implant surfacesembellished with nanoscale topographies. The goal of this review is to consider the role of nanoscale topographic modification of titanium substrates for the purpose of improving osseointegration. Nanotechnology offers engineers and biologists new ways of interacting with relevant biological processes. Moreover, nanotechnology has provided means of understanding and achieving cell specific functions.
The various techniques that can impart nanoscale topographic features to titanium endosseous implants are described. Existing data supporting the role of nanotopography suggest that critical steps in osseointegration can be modulated by nanoscale modification of the implant surface. Important distinctions between nanoscale and micron-scale modification of the implant surface are presently considered.
The advantages and disadvantages of nanoscale modification of the dental implant surface are discussed. Finally, available data concerning the current dental implant surfaces that utilize nanotopography in clinical dentistry are described. Nanoscale modification of titanium endosseous implant surfaces can alter cellular and tissue responses that may benefit osseointegration and dental implant therapy.
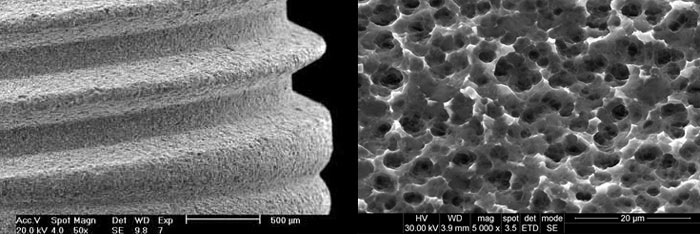
All DENTIN implants, excluding the Orthodontic screws and Provisional implants, share a total surface roughness in the boundary of 1.8-2.2 Ra microns, and a micro geometry of titanium, that is achieved by sand blasting particles and acid-etching.
A larger surface area increases the bone to implant contact, resulting in more area for bone-cell attachment. The surface topography is highly dependent on the microstructure of the titanium used. For most cell types, topography in micron and submicron ranges influence activation, adhesion, orientation, morphology, and movement of the cells. There is strong evidence that different morphological dimensions are important, and effect osteoblast interaction with the surface in different ways.
The arithmetic average of the deviation Ra is the most commonly used measurement for surface roughness. The micro geometry of DENTIN implants meets the roughness recommended in the international literature. The arithmetic average of the deviation Ra is the most commonly used measurement for surface roughness.The micro geometry of DENTIN implants meets the roughness recommended in the international literature. The arithmetic average of the deviation Ra is the most commonly used measurement for surface roughness.